Social Connectedness is a Social Determinant of Health

Sometimes, in the middle of talking to someone, I start to wonder about their social support networks…”does he have someone to call when he needs to talk?” and “would she have the support she needed after surgery?” I’ll be a in a room and find myself looking around, just wondering if most people are doing ok, or who could use extra support. And I am always struck by how much I don’t know, how I can’t tell by looking at anyone, what kind of social support they have. This matters, as social connectedness is a social determinant of health. Here’s what I mean.
We are all embedded in social support networks, but they are largely invisible, not only to ourselves, but also to the people who care for us. Social connectedness is a social determinant of health. It’s one of the biggest predictors of health and well-being, but also one of the hardest to measure, understand and detect.
My Mom Demonstrates that Social Connectedness is a Social Determinant of Health
This lesson became profoundly real to me about 6 years ago. I remember sitting in the office of my mom’s oncologist one day for her weekly check-in during her 7th round of chemo, and he asked her a simply normal question, “how are you doing Maggie”? She talked about her always present neuropathy and weakness from the chemo, but this time she also told him that she was starting to have trouble with her mobility, especially getting up the stairs, and that even making meals was becoming too hard.
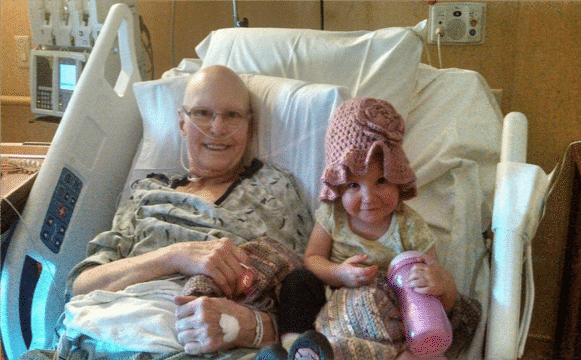
Not surprisingly, he asked her if she had anyone to help and she answers that yes, she had three adult daughters in town. He was satisfied and moved on to the rest of the checkup.
What he didn’t do was ask her the next questions “do your daughters coordinate care for you” and “do you trust them to help you when you need it”? Had he done that, he might have found out that two of us are estranged and another daughter’s husband had just had a debilitating stroke and was in the ICU at that moment. In fact, this was the first time I was hearing my mom talk about these things and I knew in that moment that she wasn’t getting the help she needed. But her lack of social support, her reality of being mostly socially isolated, was completely unknown to her oncologist.
In the end, she made many poor health choices, probably because she didn’t have a coordinated network of supportive people around her. It’s not an easy thing to think about. And I am certain that her adverse social connectedness impacted her health outcomes. Like so many others who suffer from social isolation, or other types of adverse social connectedness, she may have survived or had at least lived a happier, healthier end of life experience had things been different.
Technology Can Help Us Make Invisible Social Support Visible
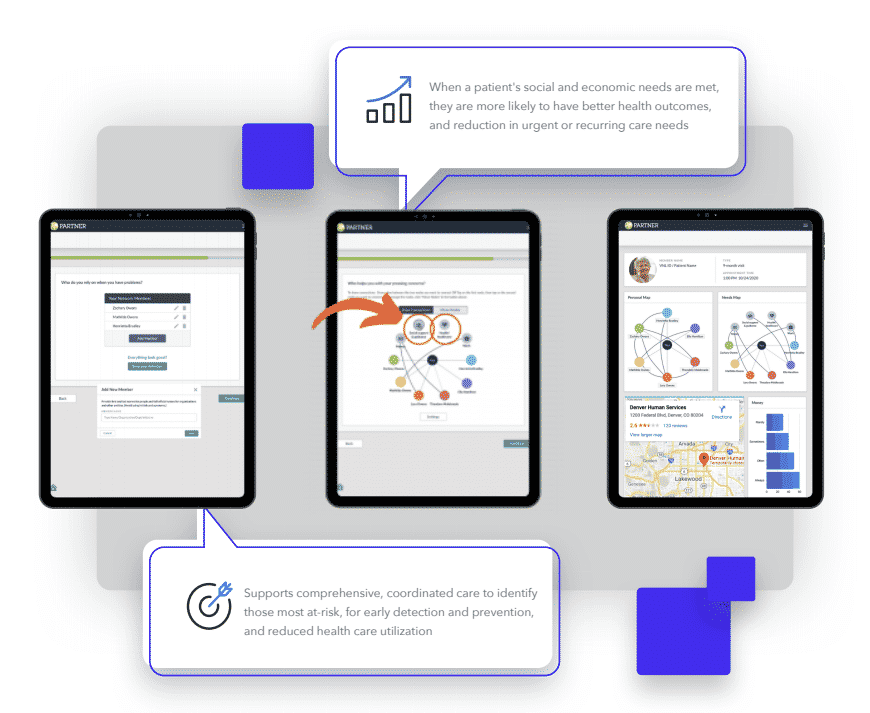
I have spent the better part of the last two decades of my life devoted to this issue, building tools and technology, data systems, and information to guide decision making and support, for helping professionals who are deeply embedded in trying to find ways to help people who are struggling. Today I’ve turned it all into a powerful data machine that we call Aspen, a reference to the symbolism of the roots of the Aspen tree and their constant interconnectedness. Aspen holds all of the hopes, dreams, and years of work that our team keeps close, as we work together to play our part in addressing this important issue.
And even as I’ve worked to build tools to put into the hands of providers, teachers, fire fighters, and social workers, to “see” the social support systems of people, I fell victim to the challenges of this deadly issue. When my mom was going through her last six months, I was starting the work to build PARTNERme – a patient engaged tool that gives people a new voice in how they can describe and show their social connectedness.
And yet, even I didn’t know how to help my mom. I often think, if I didn’t know, and I think about this stuff ALL THE TIME, how will anyone know?
I think we can do better. This is an issue that no one person, no one program, no one solution can fix alone. We all have a role in solving this problem. We need to ask ourselves, “what is MY call to action?” How can I use my special skills, my own experiences, and my own thinking to help address this invisible, crucial issue?
As a network scientist, I think about this issue in a very specific way. I was lucky enough to learn this way of thinking 20 years ago, and quickly became obsessed with knowing that this could be one way that I could help connect people to people, organizations to organizations, and people to organizations.
My Call to Action to Improve Health & Well-Being
People are so varied in the ways in which we have social connectedness, or do not. Network science gives us tools to visualize and detect ways to know which of us are strong, or where we struggle. I’ve noticed we have narrowed much of this conversation of the concept of social isolation. Yes, social isolation is an intractable problem, and is the culprit of many adverse outcomes. But it is only one kind of adverse social connectedness – we can be connected to a lot of other people, embedded in a rich network of connections to others – and still feel lonely or isolated. We can be connected to people who abuse us, who are also users, who depend on us for everything.
As a society, we have settled on two primary ways of thinking about this:
- We have settled with tackling social isolation, because tackling adverse social connectedness is just too hard. It’s hard to understand, it’s an invisible characteristic of a person, and it is far easier to understand and see that someone is socially isolated.
- We are not equipped to understand this issue. Helping professionals are ok asking “do you have someone to talk to?” or “is there someone you trust?” but are reluctant to push further, dig deeper, and find out more. Besides that most people will simply answer yes to be a good patient, these questions hardly scratch the surface of what the true issues are for people.
Social Connectedness is a Social Determinant of Health. Now What?
With this context, we continue to try to build the ideal system of resources for people. Yet, the variations that people present and the vast amount of differences in social support systems, make the likelihood of building the “perfect” system very unlikely. Rather, if we build adaptable systems that can learn to respond to the variations that people present, and wrap those resources around people based on increased visibility on their strengths and weaknesses, we can begin to meet people where they are.
To build these kinds of systems, we need two things:
- More visibility and understanding of the variations of people’s social support systems.
- A way to track that information and respond to it in a person-centered way.
In all these years of thinking deeply about this issue, sometimes regretfully, sometimes overwhelmed with curiosity, I am motivated now more than ever to push forward on bringing visibility to this issue, building adaptable systems that can respond to the differences in people all around us, and to fulfill my call to action.
I encourage us all to ask “What’s MY call to action?”, because together we can fill in the gaps and bring visibility to adverse social connectedness. To learn more about the Person-Centered Network App and how it can help visualize support networks, click here.
About the Author: Dr. Danielle Varda
CEO, Founder, Professor, & Mother of Three Spirited Girls
Danielle is a scientist turned start-up founder, leading Visible Network Labs as CEO. Her combination of 20 years as a network scientist studying social connectedness and health, published author, 12 years as a tenured professor at the University of CO Denver, and her successful launch and scaling of the Center on Network Science came together in one big idea to start VNL. She is an entrepreneur, technologist, network scientist, fundraiser, and mother to three spirited girls. Her calling came when she realized her unique ability to develop technology solutions bridge complex systems science with everyday applications in communities, organizations, and business. She is a nationally known expert and keynote speaker on applied network science, with specific expertise in health system, public health system, entrepreneurial ecosystems, and educational system approaches. Danielle has published over 30 peer-reviewed articles on networks and their impact on health, well-being, and economic outcomes. Danielle leads VNL’s strategic partnership approach, is the company’s lead fundraiser, and has a vision for how to utilize network science to solve our most pressing and intractable problems.
In addition to her leading VNL, she is also an Associate Professor at the School of Public Affairs, University of Colorado Denver where she is Co-Director of the Center on Network Science, Director of the Nonprofit Concentration in the MPA program, and Advisor to the Dual MPA-MPH Degree. Additionally, she holds a secondary appointment in the Colorado School of Public Health, Department of Health Systems, Management, and Policy. She also has a courtesy Associate Professor appointment in the School of Information Sciences at the University of CO Boulder.
|
|
Thank you for Signing Up |

More Social Care Resources