The increasing recognition of health-related social needs (HRSNs) as critical drivers of health outcomes has spotlighted the importance of innovative approaches to identify and address these needs, especially in underserved communities.
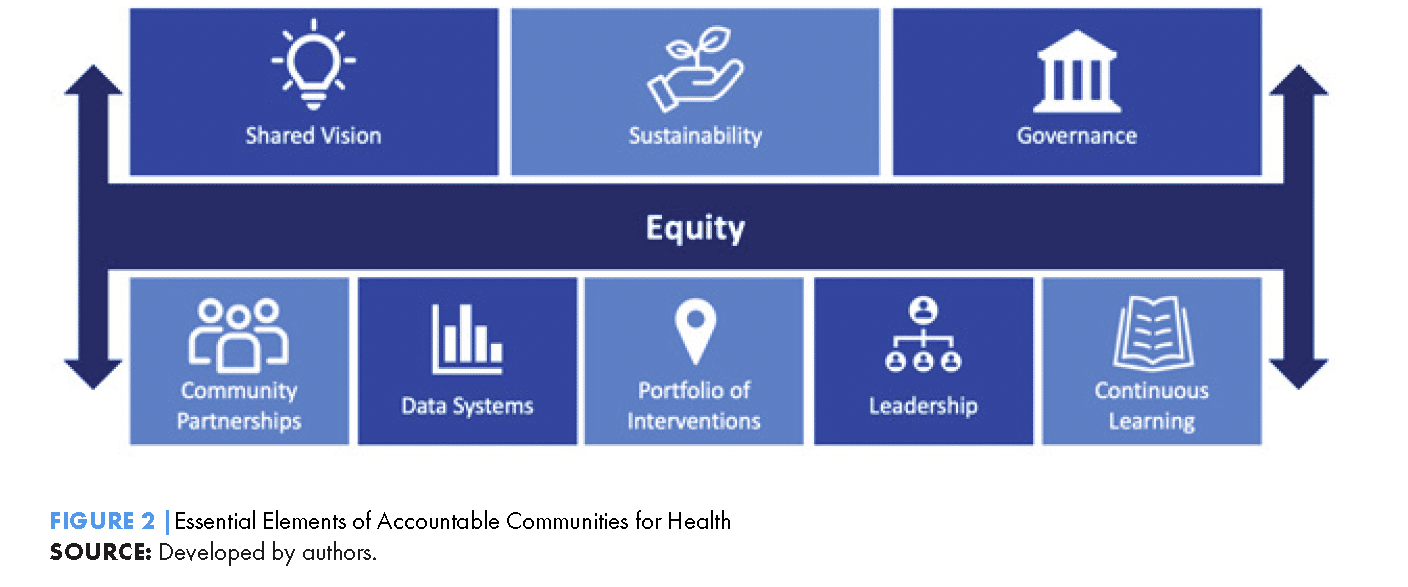
A recently published research article in Health Promotion Practice reflects on the implementation of the Accountable Health Communities (AHC) Model, a comprehensive initiative funded by the Centers for Medicare & Medicaid Services (CMS) Innovation Center.
The study highlights practical strategies for overcoming challenges in implementing HRSN screening in clinical settings, presenting valuable lessons for health systems and practitioners aiming to enhance patient well-being.
Key Insights from the AHC Model
The AHC Model screened over 1.1 million patients for critical HRSNs, such as food insecurity, housing instability, and lack of transportation, from 2017 to 2022. Notably, over 137,000 patients were connected to navigation services designed to link them with resources to address these needs.
This large-scale effort was complemented by rigorous monitoring and data collection, revealing challenges and best practices in embedding HRSN screening into healthcare workflows.
Major Implementation Challenges and Responses
Here were some of the main roadblocks and proposed strategies for overcoming them through the AHC model:
1. Engaging Patients in Screening
Patient engagement emerged as a top challenge throughout the implementation period. Patients’ comfort and trust significantly influenced their willingness to participate in screenings.
- Strategies: Awardees used culturally tailored language and outreach methods to build trust. Personalized scripts, reflective of staff personalities, made communication more natural and relatable. Community-informed script adaptations, such as using terms like “entitlement” instead of “help” for older adults, showed promise in increasing engagement.
2. Staff Buy-In and Retention
Generating buy-in among clinical staff was a critical hurdle. Without dedicated roles, staff often found it difficult to prioritize HRSN screening amidst competing responsibilities.
- Strategies: Communicating the impact of HRSN screening through patient testimonials, videos, and newsletters highlighted the tangible benefits of this work. Additionally, creating opportunities for peer collaboration, such as cross-site meetings and shared learning platforms, boosted morale and screening rates.
Get our monthly newsletter with resources for cross-sector collaboration, VNL recommended reading, and upcoming opportunities for engaged in the “network way of working.”
3. Technological Innovations During the Pandemic
The pandemic forced rapid shifts in screening methods as in-person workflows were disrupted.
- Strategies: Awardees leveraged technology, including texting, patient portals, and email campaigns, to expand screening capacity. Texting emerged as particularly effective, with tailored messages driving higher engagement. The Denver Regional Council of Governments’ email campaign also highlighted the importance of integrating trusted provider branding to build credibility.
4. Workflow Integration and Efficiency
Embedding screening processes into existing clinical workflows proved essential for scalability.
- Strategies: By involving staff in designing workflow-integrated solutions, organizations ensured that screening became a seamless component of patient registration, triage, or discharge processes. Some sites also employed interns or added dedicated staff roles to handle screenings more efficiently.

Broader Implications for Health Systems
This study underscores the value of systemic approaches to address the social determinants of health. Integrating HRSN screening into clinical practice aligns with recent CMS rules and National Committee for Quality Assurance (NCQA) guidelines, emphasizing the importance of addressing patients’ social contexts in care delivery.
Actionable Recommendations for Health Organizations
- Tailor Screening Approaches to Community Needs: Conduct focus groups and journey-mapping exercises to understand patient preferences and concerns. Use this information to refine scripts and outreach methods.
- Invest in Staff Engagement and Training: Equip staff with cultural competency skills and regularly share success stories to reinforce the value of their work.
- Leverage Technology for Accessibility: Expand remote screening options through texting, patient portals, and emails, ensuring accessibility across diverse patient populations.
- Foster Collaboration: Build connections among clinical staff through regular meetings and shared learning opportunities to exchange best practices.
- Monitor and Adapt Processes: Use performance dashboards to identify gaps, test new strategies, and optimize screening workflows.
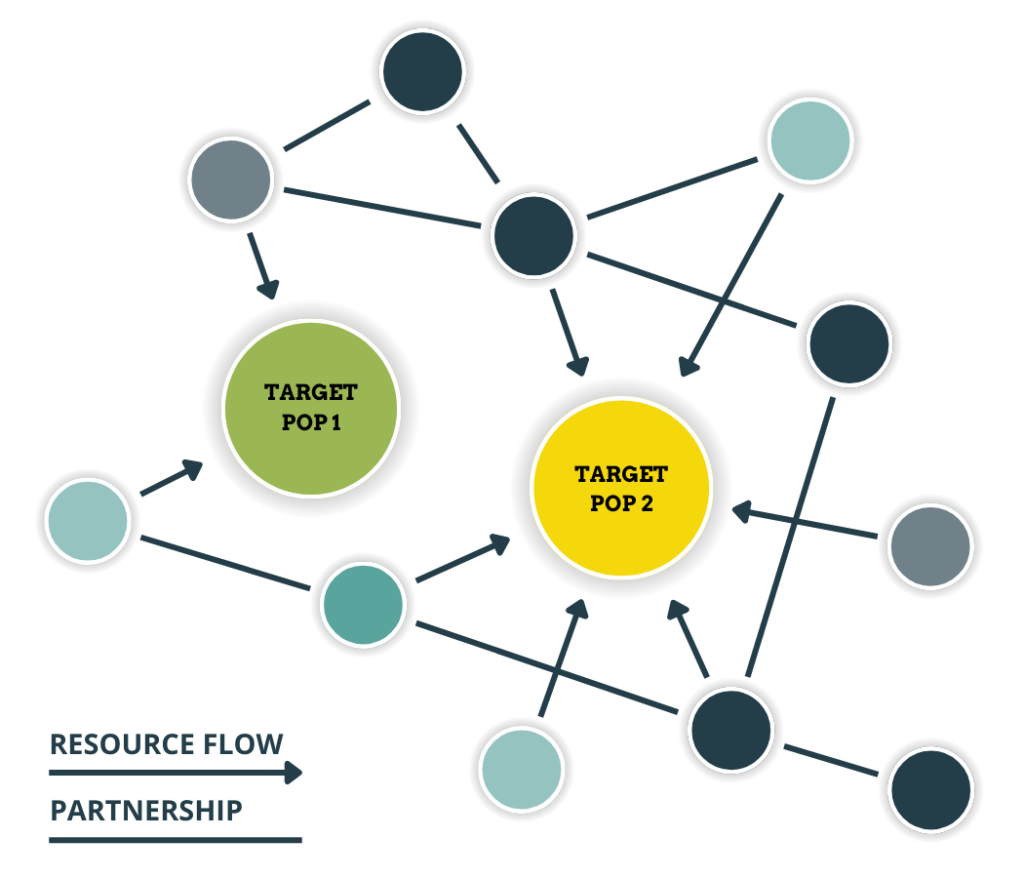
Applying SNA to Advance System Strategies
To take these strategies further, organizations can leverage tools like the PARTNER Community Partner Relationship Management (CPRM) platform. PARTNER CPRM™ helps health systems and community organizations map, analyze, and strengthen networks addressing HRSNs by fostering collaboration, tracking resources, and measuring impact.
By aligning with the recommendations from the AHC Model, PARTNER CPRM™ provides a comprehensive framework to build trust, improve workflows, and ensure equitable resource distribution.
Looking Forward: Building Sustainable Solutions
Addressing HRSNs requires not only effective screening but also the availability of resources and upstream interventions to tackle structural inequities. Sustainable success hinges on value-based payment models and robust partnerships between payers, providers, and community organizations.
The insights from the AHC Model offer a roadmap for health systems to better meet their patients’ needs and address disparities. By prioritizing patient-centered approaches, leveraging technology, and fostering collaboration, the healthcare sector can move closer to a future where social needs are seamlessly integrated into the care continuum.
Click here to read the full published article and more related research.
Take the Next Step: See PARTNER Live!
Learn more about how PARTNER CPRM™ can empower your team to create meaningful connections and drive transformative change in your community here.